No out-of-pocket expenses for hospital confinement. Free medical consultations and medicines.
It was an announcement met with cheers, sighs of relief and expectations. President Ferdinand Marcos Jr. knew how to catch the public’s attention and earned ‘pogi’ points during his fourth State of the Nation Address in July with this declaration.
Never mind if it was a rebranding of programs offered by the Philippine Health Insurance Corp. (PhilHealth) supposedly already in place and being implemented, albeit on a limited scale.
For many Filipinos, who under the Universal Health Care law (R.A. 11223) are covered by the state health insurer, these were mostly unheard of. While there have been few who have availed of the services, majority (especially those who pay monthly premiums) are unaware of such benefits and have been grumbling in dissatisfaction.
Marcos touted that when confined, patients need not worry about their hospital bills. What was previously known as the No Balance Billing (NBB) policy has been rebranded as Zero Balance Billing (ZBB). PhilHealth, the president said, would assume all costs – confinement, treatment, medication, doctor’s fees.
What he left out was that the benefit is only good when admitted to one of the 87 government hospitals under the Department of Health (DOH) across Luzon, Visayas and Mindanao, and only when confined in a basic or ward accommodation.
A basic ward means multiple patients (minimum of 3, maximum of 8) sharing a room, in a space only with fan ventilation and a common toilet and bath.
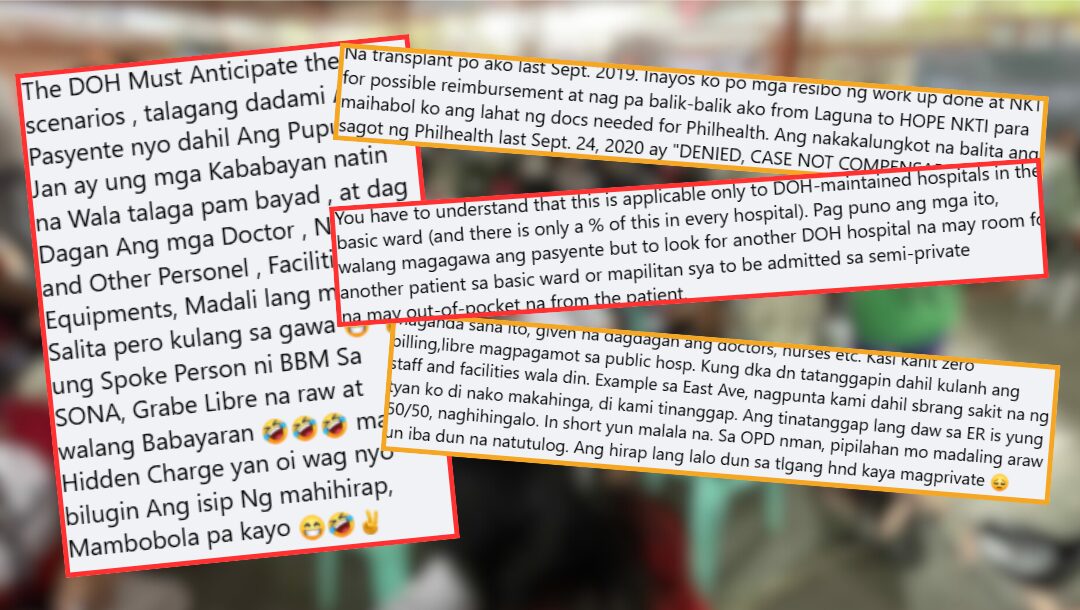
Specialty hospitals like the Philippine Heart Center, National Kidney Transplant Institute (NKTI), Lung Center of the Philippines and the Philippine Children’s Medical Center are not among the 87. These medical facilities operate as government-owned and controlled corporations (GOCCs), have their own accounting processes and are not, as of yet, linked to the DOH hospital system.
Certain PhilHealth benefits apply when treated and confined in these health facilities, but patients cannot expect zero out-of-pocket expenses upon discharge. Reduction in hospital expenses come by way of endorsement or guarantee letters from local government units, politicians and government agencies like the Department of Social Welfare and Development.
Begging for scraps
“Sa mga nagda-dialysis: Ang mga sessions ninyo na tatlong beses sa isang linggo, libre na sa buong taon. Libre na rin po pati ang mga kinakailangang mga gamot (For those undergoing dialysis: Your thrice a week sessions will now be free for the entire year. Your essential medicines will also be free.)” Marcos declared.
Maria – mother and carer of a 32-year-old with chronic kidney disease – attests that her son is covered by PhilHealth for dialysis sessions under its Z Benefit Package. This is a big deal considering the cost of dialysis.
Excluding complication-related expenses, the fees range from PHP 44,610.36 to P116,590.24 for non-diabetic patients and P46,451.88 to P120,948.12 for diabetic patients, annually.
But the Z Package for Peritoneal Dialysis (PD) covers only that. If the patient suddenly needs confinement for another illness or complication, unless admitted to a DOH hospital ward, the ZBB does not apply.
When Maria’s son needed to be admitted, the NKTI said they were not eligible for basic ward services and had to settle for a semi-private accommodation.
“Ayaw kasi kami tanggapin sa free ward. Kaya napilitan kami sa private ward (They don’t want to accept us in the free ward, so we were forced to get admitted to a private ward),” Maria related, but failed to add why they were rejected although she claimed neither she nor her son had any source of income.
Even that was a challenge because they had to secure a referral from a doctor to even be attended to. Fortunately, the employer of the patient’s older sibling knew of a doctor at the NKTI, who wrote a referral letter to prioritize admission.
Upon discharge after several months of confinement, their total bill was only discounted based on applicable case rates provided under PhilHealth, a paltry amount. Maria still had to rely on, and beg for Guarantee Letters (GLs) from politicians to settle their bill, so her disappointment and frustration are understandable and not uncommon.
Luck of the draw
Under its previous iteration NBB, coverage was limited to indigents, sponsored, senior citizens, lifetime members and domestic workers. With the UHC Act in place, all Filipinos are supposedly entitled to ZBB.
In November 2024, Rhea, a young mother whose child was confined at the San Lorenzo Ruiz General Hospital was worried about hospital expenses. Her child, diagnosed with nephrotic syndrome (damage to small blood vessels in the kidney) was treated for 13 days.
To her complete surprise, the doctor told her they were not being charged for the confinement. San Lorenzo Hospital in Malabon is one of the DOH-run hospitals.

“Iniisip ko talaga paano yung mga gagastusin namin sa ospital kasi wala rin ako[ng] trabaho. Tapos nung nakausap kami ng doctor, sabi sa amin wala daw kami babayaran. Dumating na yung bill, zero na talaga (I was thinking about hospital expenses since I had no job. When we spoke to the doctor, he said we were not being charged for the confinement. And when the billing came, it was really zero)”.
Other than assuring Rhea they would not be charged for the hospitalization, her doctor gave no other explanation. “As in zero, at wala kaming nilabas kahit piso. Kasi kahit lab test at mga ultrasound, x-ray na ginawa sa kanya, wala talagang bayad (As in zero, we didn’t spend even a peso. For lab tests, ultrasound and x-ray, we didn’t have to pay anything)”.
Through a video clip that aired on news channels and circulated on social media, Health Secretary Teodoro Herbosa used the case of a maintenance worker from Metro Manila, who underwent multiple surgeries at the Eastern Visayas Regional Medical Center (EVRMC) in Tacloban City, as proof the ZBB program works.
A victim of stabbing while on vacation, Rico Ligo incurred a bill of nearly P450,000. His daughter, Rica, attested on camera that they walked out of the hospital without spending a single centavo after PhilHealth shouldered the cost under their case rate packages, while the Department of Health assumed the balance of P372,561.44.
That the DOH paid for the bulk of the medical expense is also misleading when Marcos claims it is the state insurer that solely provides for this benefit. But this explains why only DOH-operated hospitals can offer ZBB, now dubbed as the “Bayad na Bill Mo” or BBM.
EVRMC, based in a Romualdez-Marcos bailiwick, was also hailed for having extended zero balance billing to 12,357 patients as of July 2025.
Not a warm embrace
Health authorities are now pushing for primary health care to significantly decrease the government’s burden for healthcare and hospitalization. PhilHealth has rebranded its Konsulta program into YAKAP (Yaman ng Kalusugan Program), claiming it now has more healthcare providers.
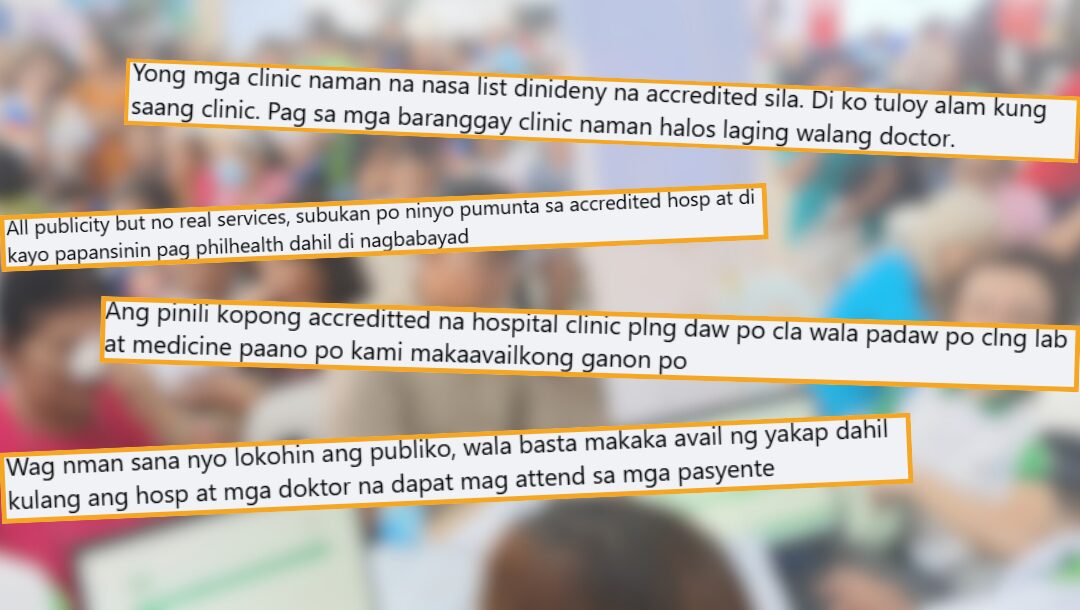
But Konsulta’s weakness of being unable to accommodate as many patients due to a lack of physicians and health centers is the same problem faced by YAKAP. At least based on member experiences shared online via comments on most PhilHealth posts.
And with a shift to online apps, specifically the eGov.ph and PhilHealth portals, there is an added challenge for members even when the intent is to facilitate ease and convenience in availing of the services.
Registering is pretty straightforward, but can be a problem for people who are technologically-challenged, or those finding it difficult to access the online sites due to weak connectivity in their area or lack of funds for data. There is still the option of personally registering at the nearest PhilHealth office.
The agency’s pronouncement of additional YAKAP providers did not seem to make a difference. There are still long queues, resulting in hours of waiting, or worse, there is no doctor to see the clients.
Walk-ins for consultations are discouraged. Scheduling an appointment via the portals is just as frustrating because the list is backed up for weeks or months. Both cause members to doubt if PhilHealth’s programs and benefits are for ‘every Filipino’ as they claim or only for a select few.

Several members who registered with YAKAP centers and were expecting to be served after continuous publicity by the state insurer had common complaints: 1) the health center, clinic or hospital is unaware of being included as a YAKAP provider; 2) there is a lack of doctors for consultations, or they fail to show up to see patients scheduled for the day 3) there is limited time to see patients; and 4) PhilHealth has yet to give guidelines for the program implementation.
First-hand experience
This writer went through the motions of registering and scheduling an appointment for the First Patient Encounter (FPE) at a YAKAP center. I was turned away by the first clinic near our school, whose staff was clueless about PhilHealth’s YAKAP program, and kept ignoring my questions.
Before I could even register at the health center near our house, I was already warned the waiting time was two to three weeks before I could be seen for the FPE. Those lined up attested to this. I came back twice, and each time there was no doctor assigned as a YAKAP provider to see clients.
Clara, a direct contributor, who followed the step-by-step process to register online and get an appointment still ended up at the hospital’s out-patient department. She was told the only coverage available under PhilHealth was the maximum annual capitation of P1,700 per member, which was apparently insufficient for her medical needs.
She was left disheartened. “Ang laki ng binabayad namin sa PhilHealth, sana naman mag give back naman sila. Ang hirap gamitin ng insurance nila. Sana wag lang sa walang trabaho magfocus ganun, magkaroon din ng magandang programa para sa mga totoong nagbabayad. (We’re paying so much for PhilHealth, I hope they give something back. It’s difficult to use their insurance. I wish they would not only focus on the jobless but also have a good program for paying members)”.

To ramp up its effort of raising public awareness for its programs, PhilHealth has been conducting caravans – among communities, local government units, schools and even local companies. The activities include YAKAP registration and FPEs with doctors on board, even the distribution of free medicines for the captive audience.
A big disappointment
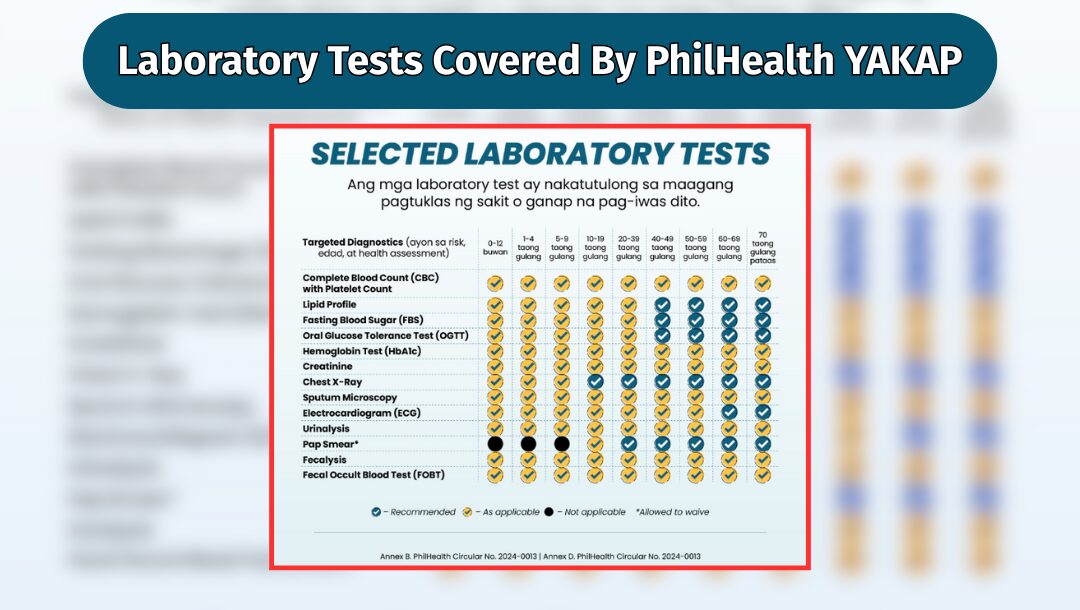
For many who have been let down by their experience of not being served by PhilHealth as promised, all the hype seems just like a huge publicity stunt. And this just for the YAKAP program, that supposedly includes 20 laboratory tests, plus cancer screening, aside from consultation.
Free medication is another clamor, especially for senior citizens, who are on maintenance medicines. And the agency’s GAMOT program, where 75 kinds of medication are included, is another disappointment.
Only prescriptions from YAKAP providers will be honored under GAMOT, even with a P20,000 annual entitlement for members. Many have complained that only very few of the essential maintenance medicines are on the list, and the more expensive ones are not.
Plus, the drugstores tied up with the GAMOT program are usually smaller pharmacies with a few branches, making it inaccessible to clients. Those who are burdened by the high cost of medicines and previously rely on health centers for these are often frustrated because of their unavailability.
If it takes a member weeks or months to be seen in a YAKAP center, how long will they need to wait to avail of the free medicines?
VERA Files has attempted for weeks to seek an audience with PhilHealth to help answer concerns raised by members. But up to this writing has been unsuccessful.
Robust collection
PhilHealth President Dr. Edwin Mercado reported that collection from direct contributors — both employed and in the informal sector — is more than satisfactory.
“This year, we’re projecting a total benefit payout of about P305 to P310 billion compared to P187 billion the previous year. So it’s actually a very hefty increase of about 88% to 90%, kumpara po noong nakaraang taon (compared to last year),” Dr. Mercado said in an interview discussing PhilHealth budget and benefits.
The national health insurer is also awaiting the return of the P60 billion out of the P89.9 billion “unutilized funds” transferred to the national treasury last year.
With the funding reverted, will PhilHealth be able to sustain the growing healthcare needs of Filipinos? For members like Maria, Rhea, and Clara, PhilHealth is more than a deduction on their payslip or a mere government support—it’s supposed to be their lifeline. But until every Filipino can access full and quality healthcare service, these programs will remain only a promise.
Editor’s note: This article was produced by a Communication Research student of the Polytechnic University of the Philippines as part of their internship at VERA Files.