A misleading article from 2018 with a headline saying consumption of coconut oil can eliminate “93%” of “colon bad cells” in two days has recently been resurrected and shared on social media. It also makes a number of inaccurate claims.
On March 14, a story titled, “Coconut Oil Removes 93% of Colon Bad Cells in Only 2 Days” — published by website Health Miracle Pedia (healthmiraclepedia.com) on Dec. 4, 2018 — was reshared on social media by at least three Facebook pages: Ian Veneracion, Jodi Sta. Maria, and Kaibigan Lang Pala. The first two pages are posing as official accounts of Filipino celebrities.
This came some weeks after the Philippine government announced that it is looking into the potential of virgin coconut oil as a treatment for the coronavirus disease (COVID-19).
The report, citing a “University of Adelaide” study as its source, made a hodgepodge of claims on colon cancer, a research on lauric acid, and the health benefits of coconut oil.
VERA Files looked into the article and found that, of the 10 claims made, only three are true. Four are misleading and three need further context.
On coconut oil and lauric acid “removing” colon cancer cells
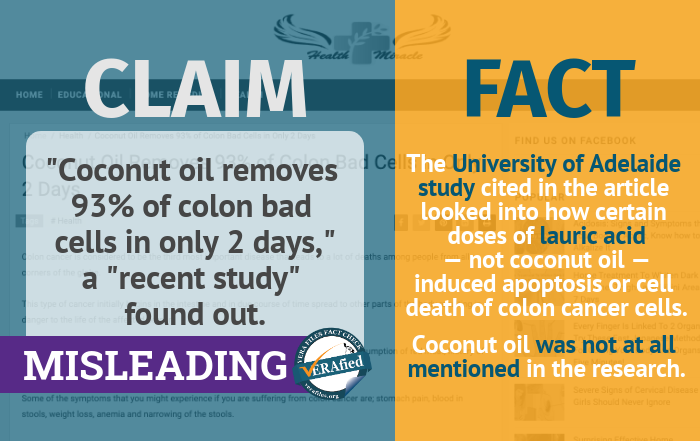
This is unsupported and misleading. The academic study cited in Health Miracle Pedia’s story made no such conclusion.
The University of Adelaide research, conducted in 2013, looked into the potential of lauric acid in inducing apoptosis or cell death of colon cancer cells. The study found that certain concentrations of lauric acid induced apoptosis in two kinds of cells used in the experiment: cultured cancer cells taken from the human colon (Caco-2), and small intestinal cell lines from rats (IEC-6).
While coconut oil does contain 80 to 90 percent saturated fat — 47 percent of this being lauric acid — the study makes no mention of coconuts. The researchers said they purchased and used sodium lauric acid from chemical and biotechnology company Sigma-Aldrich for the study.
It is wrong to claim that drinking coconut oil will have the same effect on colon cancer cells as the lauric acid used in the research, which was dispensed in calculated doses.
Oncologist Necy Juat, a member of the Philippine Society of Medical Oncology, also said in an interview with VERA Files that the potential effect of lauric acid on colon cancer cells could have been “anecdotal” and should not be treated as an alternative to medical treatment.
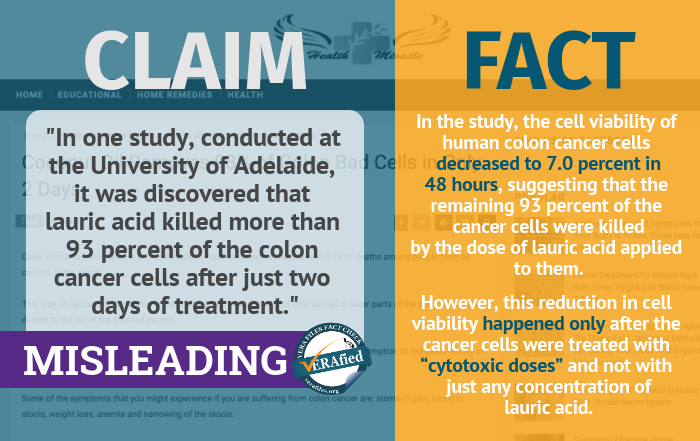 This is misleading. It was not a conclusion made by the researchers.
This is misleading. It was not a conclusion made by the researchers.
The specific finding in the study closest to Health Miracle Pedia’s claim was the significant reduction in cell viability observed in Caco-2 cells 48 hours after being treated with a “cytotoxic dose” of lauric acid.
Cell viability, in the context of the study, is the amount of cancer cells that are alive relative to the total amount of cancer cells used in the experiment. Reduction in cell viability means there are more dead cancer cells than living ones.
In the study, the cell viability of human colon cancer cells decreased to 7.0 percent in 48 hours, suggesting that the remaining 93 percent of the Caco-2 cells were killed by the dose of lauric acid applied to them.
However, Health Miracle Pedia failed to mention that the reduction in cell viability happened only after the cancer cells were treated with “cytotoxic doses.”
Cytotoxic literally means “toxic to cells.” Cytotoxic agents are substances which “kill cells, including cancer cells.” It does not only affect cancer cells, but all cells in general. Several studies had warned of the importance of proper dosing of drugs in cytotoxic chemotherapy. Underdosing could lead to “reduced effectiveness” of the treatment, while overdosing could bring about “life‐threatening adverse effects.”
Moreover, the research was performed in vitro. In vitro studies are conducted outside a living organism, usually done in a made-up and controlled environment like a test tube or a petri dish. It is misleading to assume that the results of an in vitro study would be reflected exactly in a similar, in vivo study — or that which is performed inside a living body.
Juat warned of this danger: “If you have a study in the laboratory, hindi ‘yan pwede i-translate (you cannot translate it) to a human — unless you do a phase 1,2,3,4 clinical trial. ”
Clinical trials, which usually come in four phases, are performed to evaluate the effect of new tests and treatments on humans.
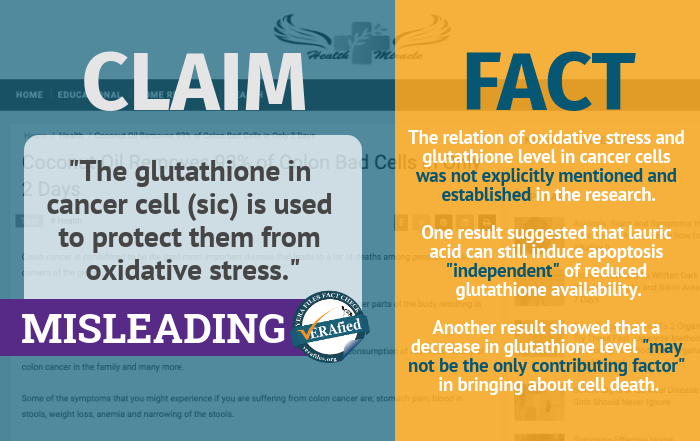
While the decrease in glutathione levels and the increase of oxidative stress were used in the study as two of the indicators of cancer cell death, the relation of the two with each other was not explicitly mentioned and established in the research.
However, the study found that higher doses of lauric acid were able to induce apoptosis in the IEC-6 cells — or the small intestinal rat cells — even without significant reduction in glutathione level. This suggests that lauric acid could still possibly bring about apoptosis “independent” of glutathione availability in the cancer cells.
It also found that lower doses of lauric acid on human colon cancer cells caused the decrease in glutathione levels “without inducing high levels of apoptosis.” This, on the other hand, suggests that the reduction of glutathione level in colon cancer cells brought about by certain lauric acid doses “may not be the only contributing factor in the induction of apoptosis,” the study stated.
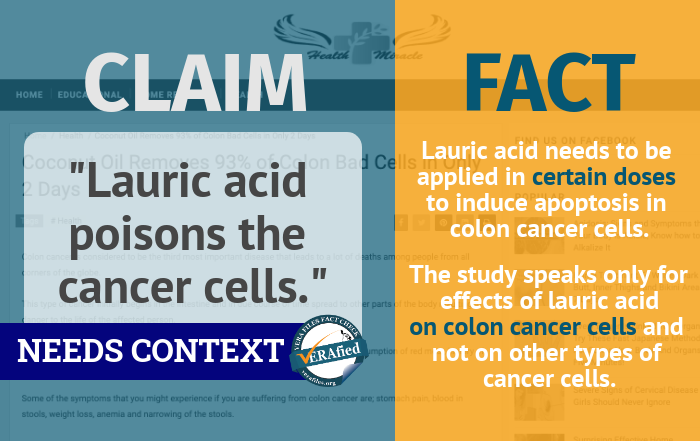
Lauric acid does not readily “poison” cancer cells in any condition. As shown in the University of Adelaide study, lauric acid needs to be applied in certain doses to be able to at least encourage cell death of — and not immediately and easily kill — colon cancer cells.
Moreover, the study speaks only for effects of lauric acid when applied to cultured colon cancer cells that are already outside of a living body.
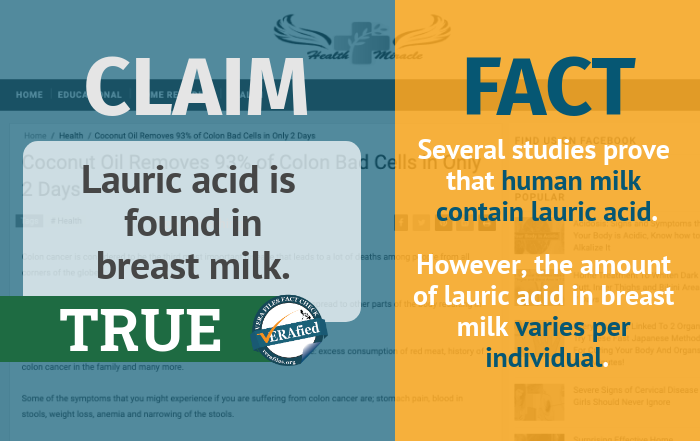
According to a 2010 study on saturated fats in mammalian milks published in the journal Lipids, human milk does, indeed, contain lauric acid. However, the amount of lauric acid in breast milk varies per individual.
A 1997 study conducted by the Oregon Health Sciences University in Portland, Oregon, published in the American Journal for Clinical Nutrition, hypothesized that there is a “rapid transfer” of fatty acids from a meal to a woman’s human milk. Fatty acids — lauric acid included — in women’s breast milk were found to increase following their consumption of formulas containing a variety of fatty acids.
On the other hand, a more recent study published in journal Nutrients in 2017, showed that the percentage of lauric acids — among other acids — in human milk changes depending on the health of both the lactating mother and her infant.
On coconut oil as a treatment to chemotherapy side effects
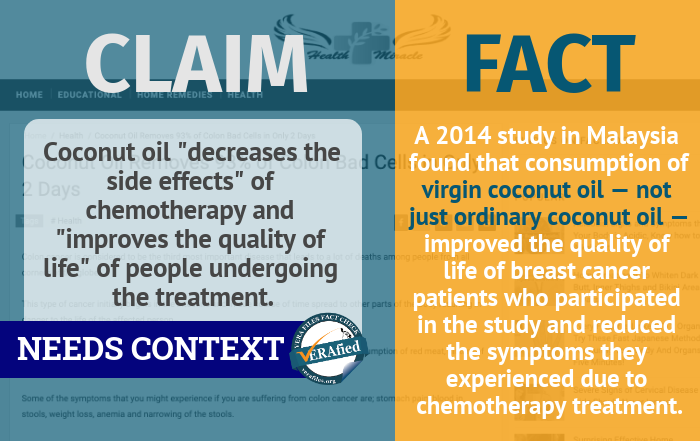 The Health Miracle Pedia article did not specify which study it used as the basis for this claim. But a 2014 study conducted in Malaysia and published in the journal Lipids in Health and Disease, found that consuming virgin coconut oil — not just any coconut oil — while undergoing the six cycles of chemotherapy treatment “improve[d] the functional status and global quality of life of breast cancer patients.” The study further concluded that it “reduced the symptoms related to side effects of chemotherapy.”
The Health Miracle Pedia article did not specify which study it used as the basis for this claim. But a 2014 study conducted in Malaysia and published in the journal Lipids in Health and Disease, found that consuming virgin coconut oil — not just any coconut oil — while undergoing the six cycles of chemotherapy treatment “improve[d] the functional status and global quality of life of breast cancer patients.” The study further concluded that it “reduced the symptoms related to side effects of chemotherapy.”
Virgin coconut oil uses fresh coconut meat, while regular coconut oil uses copra, or coconut meat that has already been dried.
On characteristics of colon cancer
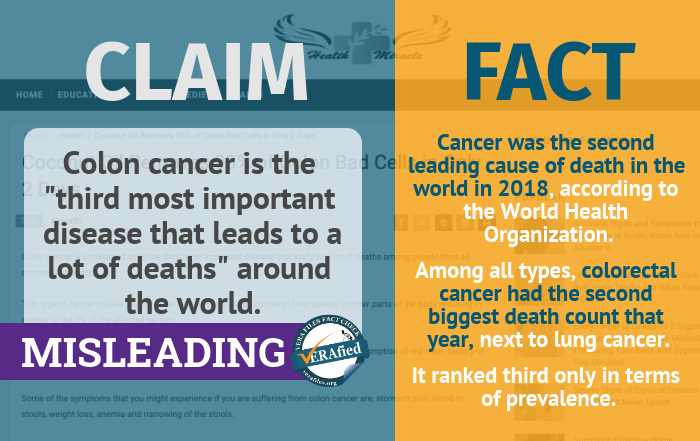
According to the World Health Organization (WHO), cancer ranks second among the leading causes of death in the world in 2018, taking the lives of an estimated 9.6 million people that year.
Colorectal cancer or cancer in either the colon or rectum is the third most common type of cancer globally, next to lung and breast cancer.
However, in terms of cancer-related deaths lung cancer holds the highest record, with 1.76 million deaths in 2018. Colorectal cancer comes in second with 862,000 deaths recorded.
Colon cancer was not among the top 10 global causes of death — which included several communicable and non-communicable diseases, and road injuries — in 2016, according to a 2018 WHO report.
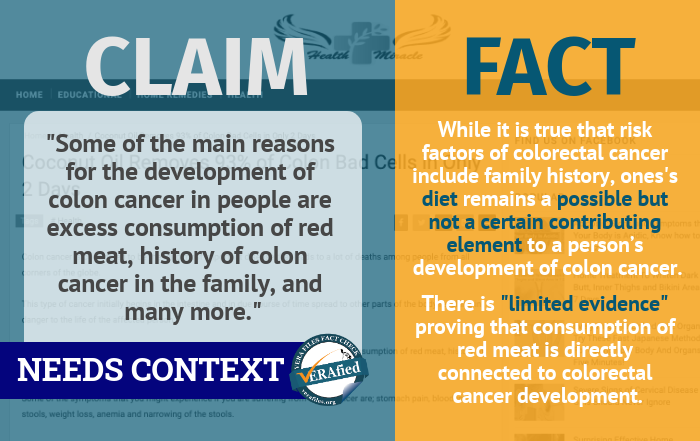
While it is true that risk factors of colorectal cancer include family history, one’s diet remains a possible but not a certain contributing element to a person’s development of colon cancer.
Additionally, there is still “limited evidence” proving that the consumption of red meat is directly connected to one’s development of colorectal cancer. The International Agency for Research on Cancer of WHO has categorized red meat as “probably carcinogenic to humans” only. While there is a “positive association” between red meat and colorectal cancer, “other explanations for the observation could not be ruled out,” WHO said.
Other known risk factors of colorectal cancer are age, personal history, inherited risk, alcohol consumption, cigarette smoking, race, and obesity, according to the United States’ National Cancer Institute.
This process is called metastasis, or when cancer cells from one organ or region of the body spread to other parts of the body by travelling through the blood or lymph system, forming a new tumor there. A cancer which has already reached distant parts of the body is called a metastatic cancer.
This is true. Aside from those mentioned, other symptoms of colorectal cancer include stomach cramps, a change in bowel habits, diarrhea, constipation, frequent gas pains, bloating, and vomiting.
Health Miracle Pedia’s article, carrying claims which have been making rounds online as early as 2014, already got more than 7,200 interactions from FB users. It could have reached over 5.7 million netizens, as shown by social media monitoring tool CrowdTangle.
Its top traffic generators since it was first shared in 2018 are FB pages Estudyante 101, Jodi Sta. Maria, and Ian Veneracion.
Health Miracle Pedia was registered as a website on June 30, 2018.

