Health authorities are cautioning the public about new cases of the monkeypox disease that have emerged in the United States (U.S.) and some countries in Europe.
“Minimum public health standards will prevent monkeypox transmission: wear your best-fitted mask, ensure good airflow, keep hands clean, and keep physical distance. These also protect us against COVID-19,” the Department of Health (DOH) said in a public advisory on May 20. As of this writing, no case of monkeypox has been detected in the country.
What is monkeypox? VERA Files Fact Check spoke with an animal virologist and an infectious disease expert to shed light on this disease.
1. What do we know about monkeypox?
Monkeypox is a viral zoonotic disease, which means the virus that causes it was originally transmitted from animals to humans.
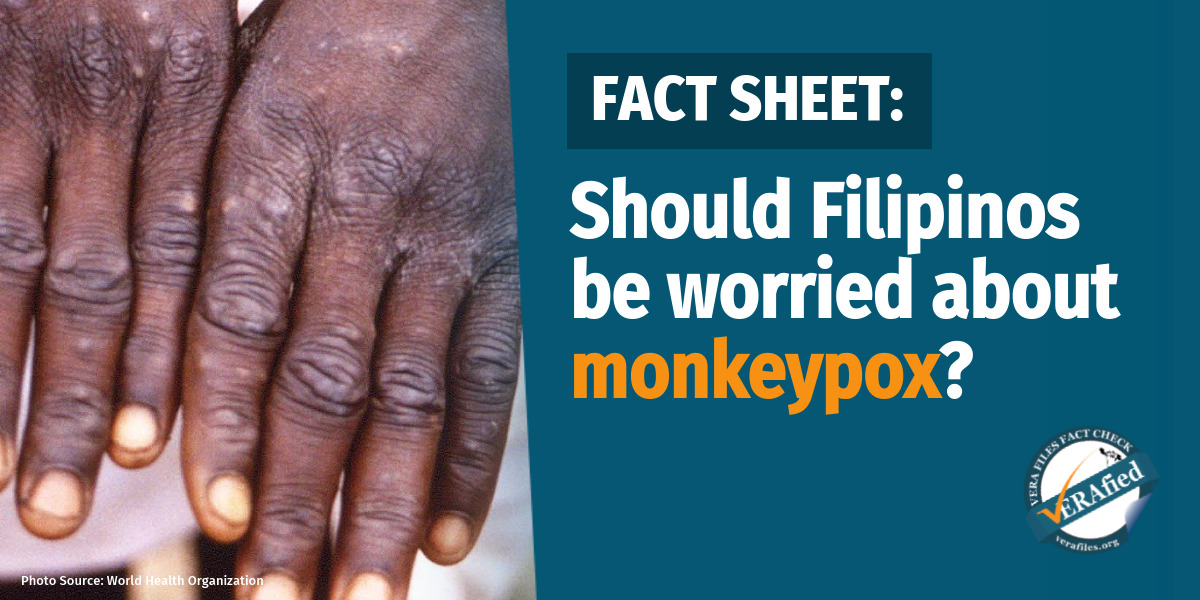
A person infected with monkeypox can spread it to others through unprotected close contact with broken skin, body fluids from skin lesions, large respiratory droplets, and contaminated materials and surfaces.
Its symptoms manifest as fever, intense headache, skin rashes, muscle pain, sore throat, low energy, and swollen lymph nodes which typically last from two to four weeks and “go away on their own without treatment,” according to the World Health Organization (WHO).
“Hindi siya ganun kabilis ang pagkalat kumpara sa COVID-19… Wala siya ‘yung presymptomatic na kahit wala kang symptom nata-transmit mo na. Kailangan close contact with the person with the lesions,” explained Dr. Marissa Alejandria, an expert on infectious diseases and professor of clinical epidemiology at the University of the Philippines College of Medicine, in a May 25 media forum.
(It does not spread fast compared to COVID-19… [Monkeypox] does not have presymptomatic indications so that even if you don’t have symptoms, you can transmit the virus. There has to be close contact with the person with the lesions.)
As of May 21, WHO has detected 92 confirmed and 28 suspected cases of monkeypox in 12 countries, including Australia, France, Netherlands, Spain, and the United Kingdom.
2. Is this a new disease?
No.
The first case of monkeypox in humans was recorded in 1970 in the Democratic Republic of Congo. It has since been classified as “endemic” in 11 African countries, mostly in the central and western parts of the continent, including Benin, Cameroon, the Central African Republic, Liberia, and Sierra Leone.
When a disease is considered endemic, it means that the epidemic level of cases has gone down but has not completely disappeared within a geographic area. (See VERA FILES FACT SHEET: When will the COVID-19 pandemic end?)
Recent cases of monkeypox were found in “non-endemic” countries where the virus has not been seen before.
Dr. Cesar Nadala, an expert on animal viruses and viral diseases, explained that zoonotic diseases like monkeypox could reappear because of international travel to countries where it is endemic, animal trade, and consumption of contaminated animal products. He said that up to now, the original animal source of the monkeypox virus remains unknown.
“Because humans are encroaching on forests where these animals are, so [there is] more contact… the more exposure we get to viruses that are normally in animals,” said Nadala, a microbiologist specializing in the creation of tests and other diagnostics.
Alejandria, president of the Philippine Society for Microbiology and Infectious Diseases, said animals associated with the monkeypox virus are the African dormouse, Gambian pouched rat, rope squirrel, and Sooty mangabey. None of these animals can be found in the Philippines, she added.
3. How is monkeypox different from smallpox?
Monkeypox and smallpox are “closely related,” Nadala said, because they belong to the same group of “orthopoxviruses” which infect mammals and humans with germs like cowpox, camelpox, and horsepox.
Orthopoxviruses are from the poxviridae family, which include viruses that cause infections “typically resulting in the formation of lesions, skin nodules, or disseminated rash.”
Here is how the monkeypox compares with the smallpox:
4. Is it preventable?
There is no specific cure available for monkeypox, but experts say it can be controlled through vaccines and treatments for other related diseases.
The smallpox vaccine can be used to prevent monkeypox since it was developed using an antigen that provides immune response to orthopoxviruses.
According to the WHO, observational studies indicate that the smallpox vaccine is at least 85% effective in preventing severe monkeypox disease.
Health authorities pointed out that there is limited supply of smallpox vaccines since the disease was globally eradicated in 1979. The WHO said it is working with manufacturers “to improve access.”
(Read VERA FILES FACT SHEET: Inside the proposed health agencies for virology and disease control)
Other antiviral treatments such as Cidofovir and Brincidofovir, Tecovirimat, and Vaccinia Immune Globulin may be used “to control a monkeypox outbreak” since they show some protection from diseases caused by orthopoxviruses or poxviruses.
However, the CDC in the U.S. noted that data on their effectiveness in treating human cases of monkeypox are limited.
5. Should Filipinos be worried?
Several health experts say the threat of monkeypox in the Philippines is “low.”
“If you don’t have close contact, you’re not going to get it [monkeypox],” Nadala emphasized, adding that the spread of the virus will likely take “a lot of time.” Nadala is involved in the research on the proposed Virology and Vaccine Institute of the Philippines under the Department of Science and Technology.
“If monkeypox is not so fatal, then you add the vaccine, and also it’s not as transmissible, so you will be able to quickly control [t]he spread,” he said.
Dr. Alethea De Guzman, director IV of the DOH Epidemiology Bureau, said the department is preparing for the possibility of monkeypox cases entering the country by “intensifying screening at borders and actively monitoring the situation.” She added that DOH is gearing up the country’s capacity for testing suspected monkeypox cases and ensuring isolation in quarantine facilities and treatment if local cases are confirmed.