For a couple of weeks two months ago, even as SARS-CoV-2 rampaged across the globe, all seemed right in the Philippines. Today, easily more than 5,000 people have tested positive for the virus all over the country and at least 300 have lost their lives. The tallies are expected to worsen in the coming weeks.
As anxiety and frustration mount, widespread testing for COVID-19 has, almost overnight, become the common call of online political commentary, a bellwether of how well (or not) a government is dealing with the crisis.
After all, as Dr Tedros Adhanom Ghebreysus, Director General of the World Health Organization, has put it, “You cannot fight a fire blindfolded.”
Last March 22, people took to the internet to echo this sentiment. Under the banner of #MassTestingNowPH, the online rally called on the government to expand its testing capacity greatly and to make the kits free. The mainstream media, too, is awash with an almost daily accounting of these kits: how many are coming in and from where, which is cheaper than which, and have we been duped into accepting substandard donations.
But testing for COVID-19 will need much more than the kits. The entire process involves so many other elements―reagents, machines, infrastructure, human resource―without which the test kits will be useless.
The clock starts ticking the moment the swabs are collected. Viruses can survive only for so long in open air before their genetic material starts to degrade. At refrigerator temperatures, shelf life can be stretched to about a week. Beyond that, however, the specimens will have to be stored at sub-zero conditions―at least –70oC, to be precise.
And so, in a race against time, a technician collects the samples―one from the throat and another from deep inside the nose, at the farthest rear wall―and dunks them into sterile tubes of a liquid called the viral transport medium. Inside a cooler full of ice, and under layers of packaging, the virus is sustained for the rest of the trip.
Back at the lab, before anything else is done to the samples, the viruses will have to be inactivated to keep the technicians safe. Heat is one way to accomplish this, according to Dr Neil Andrew Bascos, PhD, Assistant Professor at the University of the Philippines Diliman National Institute of Molecular Biology and Biotechnology. Some chemicals, particularly those involved the next step, work, too.
Viruses keep their genetic material (ribonucleic acid, in this case, instead of the typical deoxyribonucleic acid in humans and animals) sealed inside their protein-and-fat coats. These need to be cracked open before the SARS-CoV-2 testing kits can hope to detect anything.
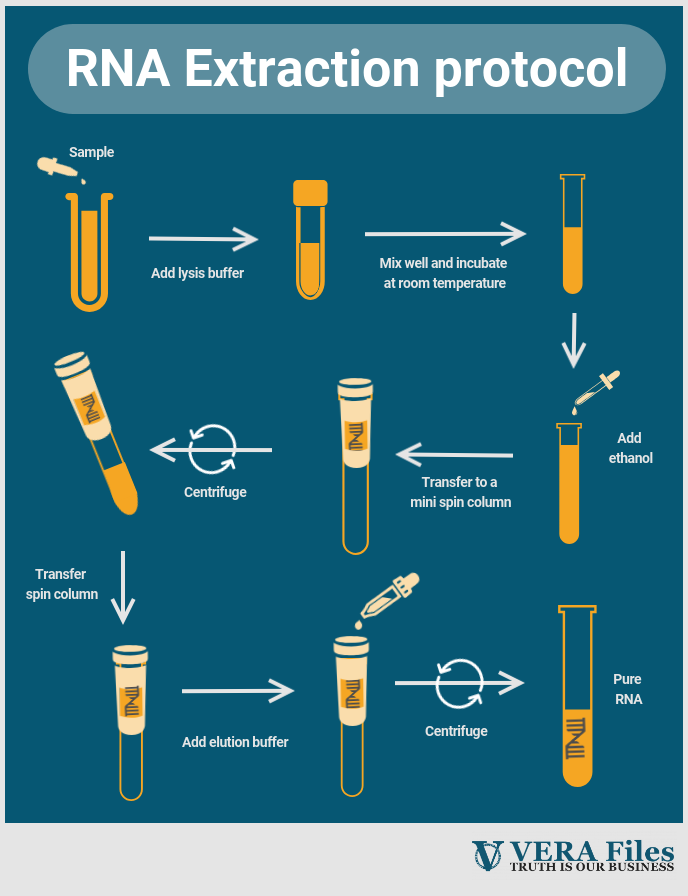
The process of isolating RNA from the samples is itself facilitated by dedicated kits. Specific details vary from kit to kit, but, generally, the goal is to open up the cells and the viral particles they contain, shut down molecules that may destroy genetic material, and sequester the RNA, away from all the other intracellular gunk.
(Kits pertain to sets of reagents that have been calibrated to work analytically well with each other. They also include inserts with directions for use. Some RNA extraction kits, for example, will have five tubes of reagents. This is also the case with the homegrown SARS-CoV-2 test kits, which contain three tubes.)
Unfortunately, getting to this viral motherlode is arguably the toughest step of the entire testing flowchart, and is a major bottleneck in the process, Dr. Bascos says. Each batch of samples up for RNA extraction, some 20 tubes or so, can take hours of work and a bagful of supplies. Even before the actual testing for SARS-CoV-2 begins, the lab will have already dug deep into its inventories.
Up until this point, the testing facility has just been preparing the samples for the actual virus detection. What results is a solution that is, in a word, messy. It will contain RNA from the virus, if present, but also from cells, from bacteria, and from whatever else was in the subjects’ throats when the swabs were collected. This is where the SARS-CoV-2 test kits come in.
These kits are based on a mainstay technique in molecular biology called polymerase chain reaction (PCR, for short), which targets a specific stretch of DNA and puts it through 30 or so cycles of DNA replication, copying it over and over. If present in the sample, PCR will have amplified the target sequence, allowing for easy detection.
But not just any PCR machine will do. SARS-CoV-2’s genetic material is RNA, not the typical DNA that the regular PCR machines usually handle. Testing centers need to use kits and machines that first reverse-transcribe the virus’ RNA into DNA, and then measure the amount of copies produced in real time, after every PCR cycle.
This process is called quantitative, reverse transcription PCR, and while the basic PCR machines are a dime a dozen in labs across the country, the machines that can pull off this more advanced technique are scarce.
It should go without saying that, at every step of the way, handlers and technicians have to be extra careful―and extra liberal with their use of disinfectants. These are highly infective viruses, after all, and the threat of contamination will always be present.
Improper handling and opening of sample tubes after heat inactivation may lead to aerosol formation, risking the infection of lab technicians, Dr. Bascos points out. The risks persist throughout the entire process, which is why testing is done in labs that are of biosafety level 2+.
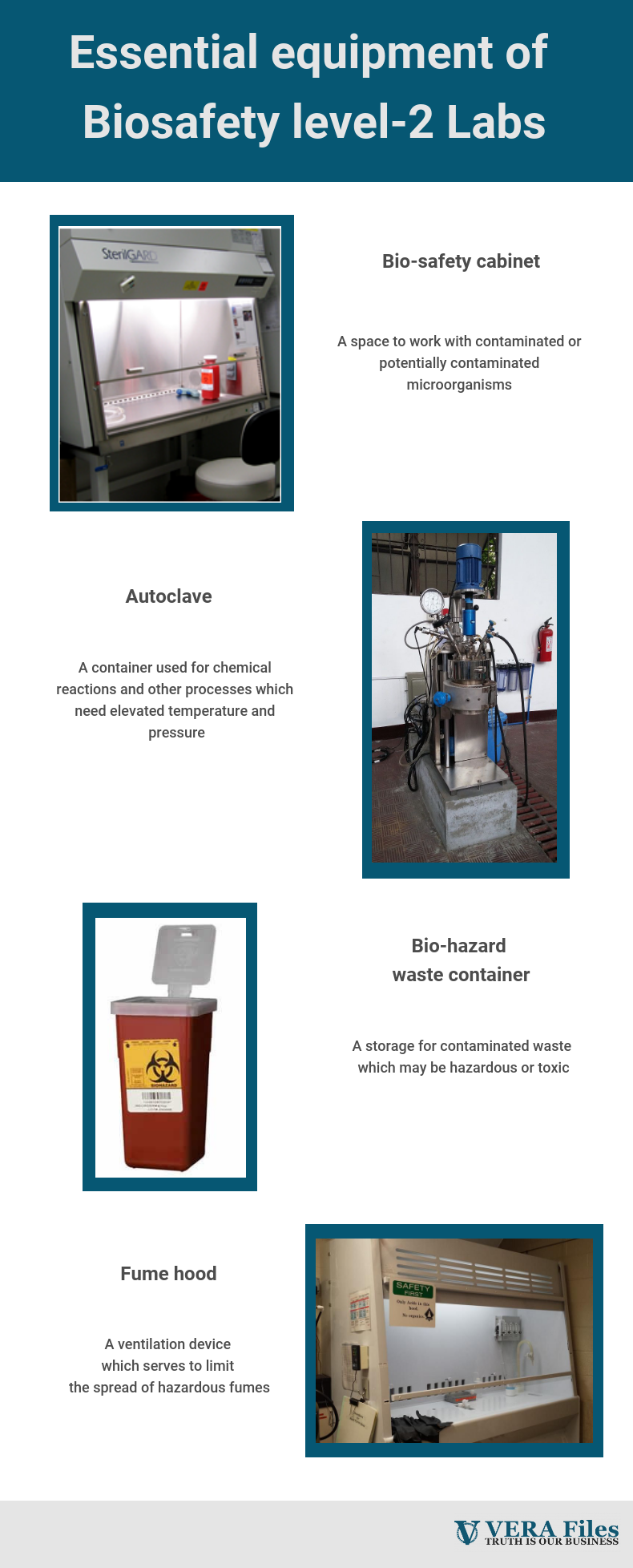
These facilities are built with the special purpose of containing threats inside. Air flow in labs, for instance, should be inward to keep aerosols and droplets from leaking out into adjacent hallways and non-lab rooms. Labs should also come fitted with sterilization equipment and biosafety cabinets, which allow technicians to safely handle potentially infectious samples.
As of even date, the Department of Health has cleared 16 labs as testing facilities. These labs have proven that they can reliably detect SARS-CoV-2 in patient samples without putting their own people at risk.
At present, while scope of testing remains limited, the threat of a broken pipeline remains far off. Labs still have their RNA extraction kits from before the health crisis, and the reserves of supplies (plates, pipettor tips, all the different kinds of tubes, among others) should still be fine.
But because demand is soaring all over the world, it may become more and more difficult for the country to maintain a secure supply chain for these essential, but often unseen, parts of the testing process. Proceeding thoughtlessly may suffocate efforts to contain the outbreak.
Dr. Bascos knows this. And so do a lot of other experts and authorities who understand COVID-19 testing holistically. On their own and in quiet collaborations, these people are trying to prepare what they can, helping the country contain a problem before it explodes into a disaster.