As the pharmaceutical industry races to find treatment for coronavirus disease (COVID-19), President Rodrigo Duterte has guaranteed that he will lift quarantine measures in the country once a “cure” is out in the market.
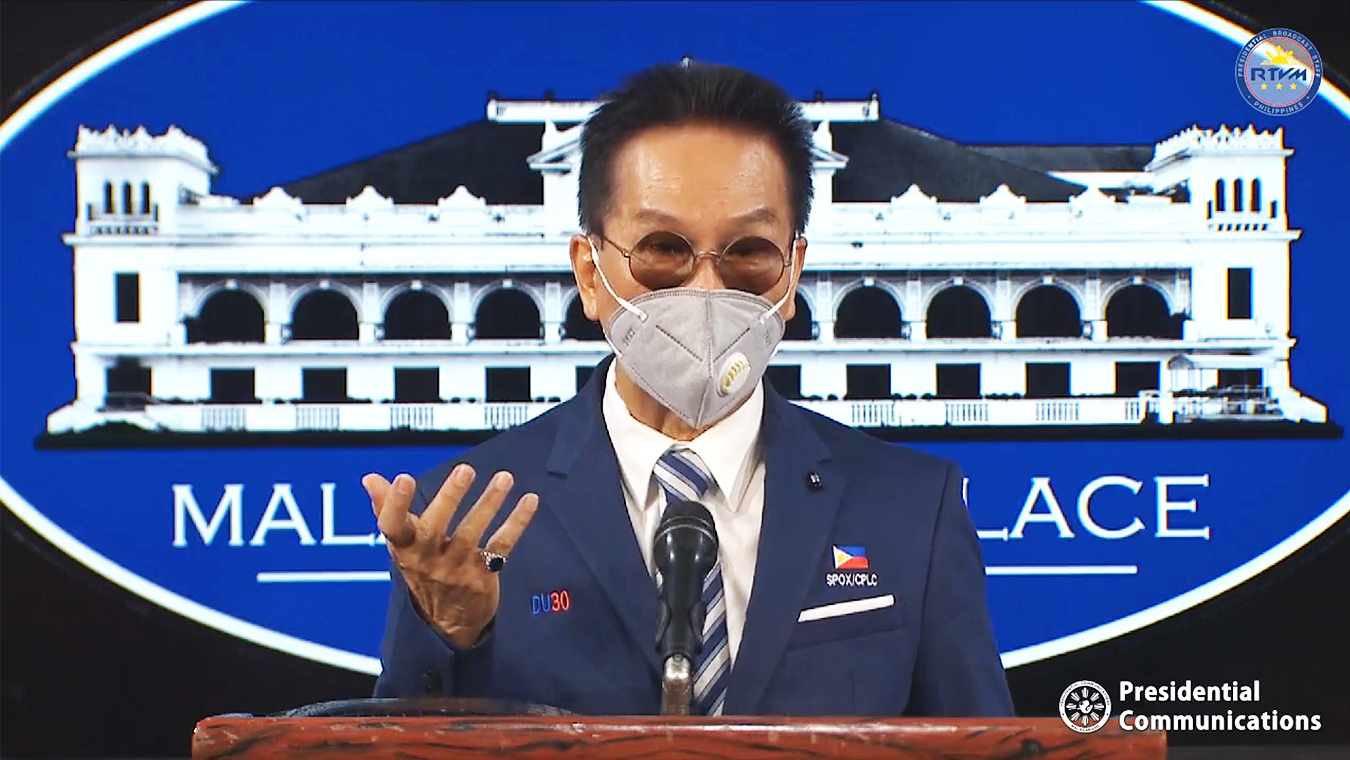
In a press briefing on April 13, the president said, while he cannot mention their names, “giant” pharmaceutical companies are now looking into “antibodies” as treatment for the disease:
“Dito sa nabasa ko…meron nang medisina, antibody ang isang giant pharmaceutical… Kung meron na ‘yan tapos makita ko na ginagamit na ng tao, ili-lift ko (From what I’ve read…there’s already a medicine, antibody by a giant pharmaceutical…If that’s already available and I see it used by humans, then I would lift [the quarantine]).”
Source: Presidential Communications Operations Office, Talk to the People of the President Rodrigo Roa Duterte, April 13, 2020, watch from 33:15 to 34:47
Duterte said the pharmaceutical firms are “racing against one another” and would “maybe” start marketing it by May.
What is an antibody and how will it help fight the COVID-19 virus?
Here are five things you need to know.
1. What is an antibody?
Antibodies are proteins produced by the immune system to help the body fight off a particular disease by “destroying” toxins or “disease-carrying organisms,” according to an explainer of the United States Centers for Disease Control and Prevention (CDC).
This will give the person a level of immunity for certain diseases. The CDC explainer identifies two types of immunity: active and passive.
2. How do antibodies help fight off an infection?
Antibodies have the ability to recognize and neutralize an antigen or foreign substance, including the COVID-19 virus (officially known as SARS-CoV-2), to prevent it from replicating itself.
When the SARS-CoV-2 enters the body — typically through respiratory droplets and into one’s eyes and nose — it attaches to, and enters, a cell. Once inside, the virus “hijacks” the cell to make more copies of itself, destroying its host in the process. The new copies of the virus then spread and infect neighboring cells, according to several explainers.
To address this viral infection, the body issues what WHO calls an immediate “non-specific innate response” to slow the progress of the virus and “may even prevent” it from causing symptoms.
This is then followed by an “adaptive response,” wherein the body generates antibodies — or proteins called immunoglobulins — that specifically “bind” to the virus. It will also produce “T-cells” that can recognize and eliminate other infected cells, WHO said in a scientific brief.
Combined, these responses “may clear the virus from the body,” and, if “strong enough,” may prevent the virus from developing into a severe illness or even reinfection from the same virus, WHO added. But while the antibody response provides “some level of protection,” the extent and duration of such protection is still unknown.
3. Are antibodies the same as vaccines?
No, they are not.
Vaccines are products that contain a “killed” or “weakened” version of the germ or virus that causes a particular disease (like COVID-19). These are then used to “train” a person’s immune system to produce antibodies so that he or she develops immunity without having to get the disease first.
They reduce the risks of getting infected by helping the body’s immune system “remember” the disease and how to fight it.
Scientists and medical experts have emphasized the need for a vaccine in order to “control” the COVID-19 virus. But a vaccine typically takes years to develop because of the tedious process it undergoes before it is declared safe and effective.
For a COVID-19 vaccine, experts predict it would take at least 12 to 18 months before it can be widely used around the globe. This is where the testing of other treatments comes in.
4. How are antibodies used to treat COVID-19 patients?
While there are currently no drugs proven yet to cure or prevent COVID-19, health care providers are looking into a number of ways on how to treat their patients, including the use of antibodies to develop passive immunity.
In the Philippines, some medical institutions, such as the Philippine General Hospital (PGH), are administering “convalescent plasma therapy” for severe to critically ill patients.
Convalescent plasma therapy is a passive immunity treatment whereby individuals who have recovered COVID-19 may donate their plasma, or the liquid part of the blood, which contains the antibodies, to help current patients fight off the infection.
The treatment is currently being used “adjunctively” with other medications, and as a “last resort” since there is “no clear-cut evidence yet that plasma therapy works,” PGH spokesperson Jonas del Rosario said in separate online interviews.
Del Rosario said PGH “plans” to look into applying the treatment to moderately ill patients to potentially prevent the further deterioration of their conditions. (See The science behind COVID-19 testing)
In its interim guidelines released on March 20, WHO said “experience suggests that empirical use of convalescent plasma may be potentially useful for COVID-19.”
5. Are there any cures, medicines, or treatments scheduled to be released in May?
So far, there is “no magic drug or known treatment for COVID-19, and there is an urgency to find effective treatment,” Health Undersecretary Maria Rosario Vergeire said in an April 16 presser.
The Philippines is one of the 100 countries currently participating in the WHO Solidarity Trial, an international clinical trial that will test the safety and effectivity of four treatment options using “investigational” drugs — medicines used in other diseases — such as chloroquine (for malaria) and hydroxychloroquine (for rheumatology), against COVID-19.
Vergeire said 500 patients will initially participate in the study, to be conducted in 20 hospitals nationwide. In an email to VERA Files, the health undersecretary said “since the trial will continue until the requisite number of subjects are enrolled, no results are immediately forthcoming.”
Meanwhile, 102 candidate vaccines are currently in various stages of evaluation as of April 30, WHO said.